PRETREAT Trial: Proactive vs Reactive Intraoperative Hypotension Management & 6-Month Disability
The PRETREAT randomized clinical trial compared a risk-stratified, proactive blood pressure management strategy to standard reactive care during surgery. In adults undergoing noncardiac surgery, it found no significant improvement in functional disability at 6 months.
Proactive vs Reactive Blood Pressure Control During Surgery: Insights from the PRETREAT Trial
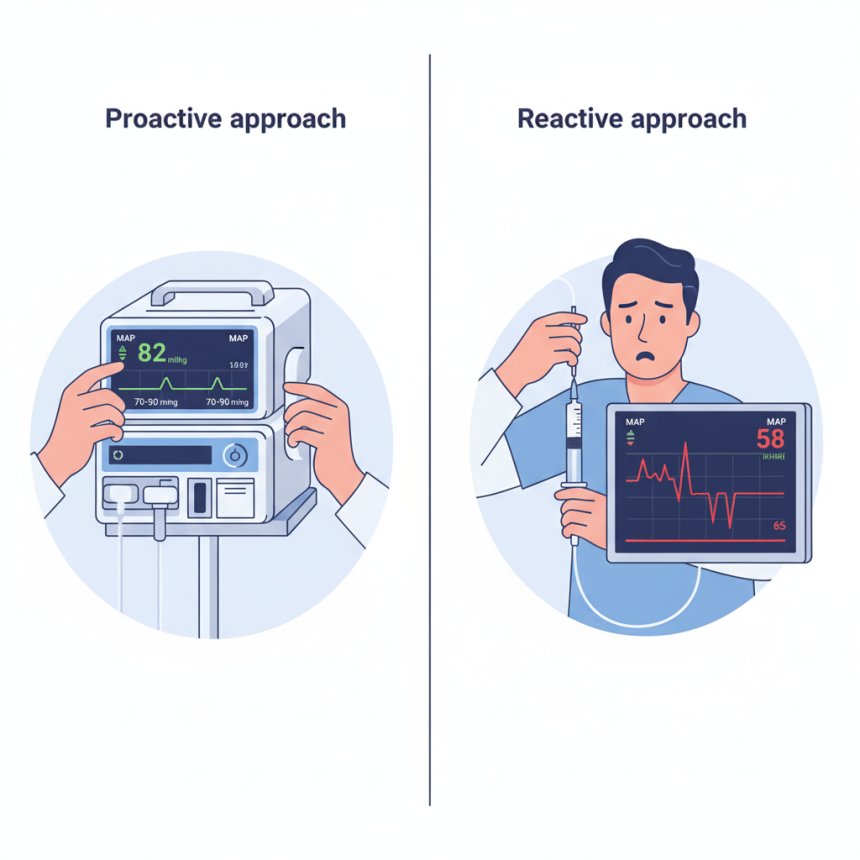
Managing blood pressure during anesthesia is a vital part of safe surgical care. However, clinicians continue to debate whether actively preventing blood pressure drops (proactive strategy) leads to better outcomes than responding to them when they occur (reactive approach). The PRETREAT Randomized Clinical Trial, recently published in JAMA (October 2025), provides important evidence addressing this question.
Study Overview
The PRETREAT trial investigated whether a proactive, risk-adjusted strategy to maintain higher intraoperative mean arterial pressure (MAP) could improve long-term recovery and functional outcomes compared to usual reactive management.
The study enrolled 3,247 adult patients undergoing elective, noncardiac surgical procedures at two hospitals in the Netherlands between June 2021 and February 2024. Participants were randomly assigned to one of two groups:
-
Proactive treatment group: Patients were managed with individualized MAP targets based on preoperative risk. The thresholds were ≥70 mmHg for low-risk, ≥80 mmHg for intermediate-risk, and ≥90 mmHg for high-risk individuals.
-
Reactive (standard care) group: Anesthesiologists maintained blood pressure using conventional methods, intervening only when MAP dropped below approximately 65 mmHg.
The primary outcome was functional disability at 6 months after surgery, measured using the World Health Organization Disability Assessment Schedule (WHODAS 2.0). Secondary outcomes included postoperative complications, quality of life, and mortality.
Findings
The trial was stopped early after an interim analysis indicated a low likelihood of significant benefit from the proactive approach.
At six months, the average WHODAS scores were almost identical between groups—17.7 points in the proactive group versus 18.2 points in the standard-care group. The difference (–0.5 points) was statistically insignificant and far below the predefined threshold for clinical relevance.
Although patients receiving proactive care experienced fewer and shorter episodes of hypotension during surgery (MAP <65 mmHg), this did not translate into improved functional or clinical outcomes. Rates of complications such as myocardial injury, kidney dysfunction, and mortality were comparable in both groups.
The proactive protocol also led to greater use of vasopressor medications, though without a significant increase in adverse cardiovascular or neurological events.
Interpretation
The PRETREAT study suggests that maintaining blood pressure above conventional targets does not enhance long-term recovery or quality of life following noncardiac surgery. While intraoperative hypotension remains a known risk factor for organ injury, these findings indicate that more aggressive correction beyond a MAP of 65 mmHg may offer limited additional benefit for most patients.
Investigators noted that the trial’s early termination and modest MAP difference between the groups (~6 mmHg) may have reduced the ability to detect smaller effects. Nonetheless, the results align with prior large trials, such as POISE-3, which found no meaningful benefit from elevated intraoperative pressure targets.
Clinical Implications
For anesthesiologists and perioperative teams, PRETREAT reinforces the principle that maintaining MAP ≥65 mmHg remains a safe and evidence-based standard for the majority of surgical patients. Pushing MAP higher should be considered selectively, taking into account individual patient profiles, comorbidities, and intraoperative dynamics.
The findings also highlight the need for personalized hemodynamic strategies, potentially guided by real-time physiology, organ perfusion metrics, or biomarkers rather than universal pressure thresholds.
Future Directions
Further research could focus on identifying subpopulations—such as those with severe cardiovascular disease or frailty—who might benefit from a more tailored blood pressure approach. Future studies may also examine outcomes such as organ-specific injury markers, neurocognitive recovery, or long-term quality of life rather than broad disability scores alone.
Conclusion
The PRETREAT trial provides strong evidence that routine proactive management of intraoperative hypotension offers no measurable improvement in long-term functional recovery after noncardiac surgery. These results support maintaining the current, well-established standard of care—intervening when MAP falls below 65 mmHg—while continuing to explore more refined, patient-centered methods for perioperative blood pressure control.
References
-
Kant M., van Klei W.A., Hollmann M.W., et al. Proactive vs Reactive Treatment of Hypotension During Surgery: The PRETREAT Randomized Clinical Trial. JAMA. Published October 12, 2025. DOI: 10.1001/jama.2025.18007
-
Kant M., et al. The PRETREAT Trial Protocol: Design and Rationale. BJA Open. 2024;9:100262. DOI: 10.1016/j.bjao.2024.100262
-
Editorial. Perioperative Blood Pressure Control and Functional Outcomes. JAMA. 2025.