AI-Guided Sperm Recovery Leads to First Successful Pregnancy in Men with Azoospermia
Columbia University researchers achieve a breakthrough pregnancy using AI-guided sperm recovery technology, marking a major advancement for men with azoospermia and male infertility treatment.
AI-Guided Sperm Recovery Leads to First Successful Pregnancy in Men with Azoospermia
Summary
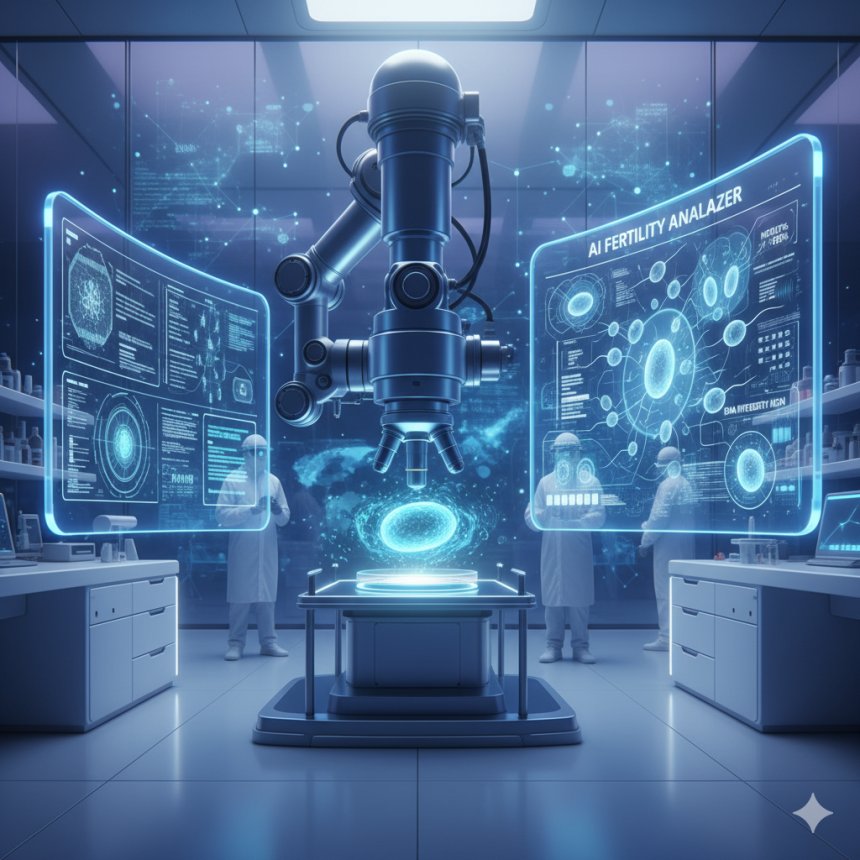
Researchers at Columbia University have achieved the world’s first successful pregnancy using an artificial intelligence (AI)-driven sperm recovery method, marking a monumental advancement in reproductive medicine for men with azoospermia—a condition where semen contains little or no sperm. The new STAR (Sperm Tracking and Recovery) technology employs advanced imaging, microfluidics, and robotics to locate and extract rare viable sperm cells, offering renewed hope for men previously considered infertile.
Key Highlights
- First successful pregnancy achieved using AI-guided sperm recovery in a patient with azoospermia.
- The new STAR (Sperm Tracking and Recovery) system can scan over 8 million images in less than an hour.
- Combines high-powered imaging, AI algorithms, and microfluidic technology for precise sperm isolation.
- Developed by researchers at Columbia University Fertility Center and published in The Lancet.
- Offers potential new treatment pathways for 10–15% of infertile men diagnosed with azoospermia.
Introduction
Infertility affects millions of couples worldwide, and nearly 40% of cases are attributed to male factors. Among these, azoospermia—where semen contains no detectable sperm—remains one of the most challenging conditions to treat. Traditional approaches, such as surgical extraction or manual searches under microscopes, are often labor-intensive, expensive, and yield limited success rates. In a groundbreaking development, scientists from Columbia University have introduced an AI-powered technique that identifies and recovers viable sperm cells with remarkable precision, offering new hope for patients struggling with male-factor infertility.
Impact on Healthcare Sector
The introduction of AI into reproductive medicine signifies a major technological leap. Columbia University’s STAR (Sperm Tracking and Recovery) method integrates artificial intelligence with microfluidics and robotics to automate one of the most intricate and time-consuming steps in fertility treatment: finding a single viable sperm cell. The impact on fertility centers could be transformative, reducing manual labor, improving accuracy, and expanding access to advanced treatment options for men with severe infertility conditions. By automating sperm identification, the STAR system also minimizes human error and increases the likelihood of successful conception through assisted reproductive technologies such as IVF and ICSI.
Effects on Healthcare Professionals
For embryologists and reproductive endocrinologists, the STAR method represents a paradigm shift in workflow efficiency. Traditionally, lab technicians spend hours manually analyzing samples under microscopes, often with minimal success. The AI-guided system, by contrast, can process millions of images within minutes, allowing professionals to focus on patient care, counseling, and treatment optimization. Furthermore, the reduction in manual intervention lowers fatigue and subjectivity in sperm detection, enabling consistent and data-driven decision-making across fertility centers. Physicians now have access to an objective, technology-assisted tool that enhances precision without replacing professional judgment.
Research Analysis and Methodology
The STAR technology, first unveiled in early 2025, was developed by an interdisciplinary team led by Dr. Zev Williams, Director of the Columbia University Fertility Center, alongside reproductive sciences expert Dr. Hemant Suryawanshi. The system leverages AI-powered imaging to scan semen samples from men diagnosed with non-obstructive azoospermia. Using ultra-high-resolution cameras, the technology captures up to 8 million images per hour, each analyzed by a trained neural network designed to differentiate viable sperm cells from other biological debris.
Once identified, a microfluidic chip—engineered with hair-like nanochannels—isolates the segment of the sample containing potential sperm cells. Within milliseconds, robotic arms extract the cells with microscopic precision, allowing them to be preserved or directly used for embryo creation. In the landmark clinical case reported in The Lancet, the AI algorithm successfully identified two viable sperm cells from a 3.5 mL sample in approximately two hours, both of which were used to create embryos. One embryo resulted in a successful pregnancy, confirming the practical viability of this advanced system.
Expert Insights and Commentary
“The field has really been challenged to find a better way to identify and retrieve viable sperm cells in men with exceedingly low sperm counts,” said Dr. Williams. “Our technology brings new possibilities for couples who were previously told they had almost no chance of conceiving a biological child.” He emphasizes that the STAR method is not just a research novelty—it’s a potential clinical tool that could redefine male infertility diagnostics worldwide.
Dr. Suryawanshi highlighted the multidisciplinary collaboration that made the achievement possible: “Our team integrated knowledge from imaging science, reproductive endocrinology, and micro-engineering. The result is a technology that bridges biology and artificial intelligence in a way that was previously unimaginable.” Both researchers stress the need for larger-scale trials to evaluate STAR’s efficacy across diverse patient populations and laboratory conditions.
Global and Societal Implications
Globally, male infertility remains underdiagnosed and underdiscussed, often carrying significant social and emotional stigma. The introduction of AI-based sperm recovery methods could normalize male participation in fertility solutions and help destigmatize discussions around reproductive health. In regions where access to advanced fertility treatments is limited, the STAR model could be adapted for local fertility centers, reducing dependency on high-cost manual labor and increasing the reach of reproductive care.
From a societal perspective, such technological interventions also raise important questions about ethical use, cost accessibility, and long-term health outcomes of AI-assisted embryos. However, experts agree that the potential to restore hope for families struggling for decades outweighs most challenges. As AI continues to integrate into fertility science, it may redefine reproductive equity—making assisted reproduction more inclusive, efficient, and personalized.
Future Outlook
The future of reproductive medicine appears poised for a digital revolution. Building upon the success of the STAR method, researchers envision AI systems capable of analyzing genetic health, motility, and viability of sperm in real time. Such developments could improve embryo selection, reduce IVF cycle failures, and pave the way for predictive fertility analytics. Columbia University’s ongoing clinical trials aim to validate STAR’s success across a broader range of patients and refine its hardware-software integration for commercial use.
If proven effective at scale, this innovation could lead to FDA-approved clinical applications, setting a global benchmark for AI-driven reproductive care. The technology may also inspire similar models in egg selection, embryo grading, and personalized fertility treatments. As Dr. Williams notes, “You only need one healthy sperm to create an embryo—but AI can help us find that one faster, safer, and with greater precision than ever before.”
Conclusion
The first successful pregnancy achieved through AI-guided sperm recovery represents more than a scientific milestone—it symbolizes renewed hope for millions of couples facing infertility. By merging artificial intelligence with reproductive biology, Columbia University researchers have transformed a decades-old challenge into a technological triumph. The STAR method not only showcases the power of innovation in healthcare but also exemplifies how AI can bridge human expertise and machine precision to redefine the possibilities of life itself.
References
- Columbia University Irving Medical Center. (2025). First clinical pregnancy following AI-based microfluidic sperm detection and recovery in non-obstructive azoospermia. The Lancet. doi.org/10.1016/S0140-6736(25)01623-X
- Interview with Dr. Zev Williams and Dr. Hemant Suryawanshi, Columbia University Fertility Center.
- World Health Organization. (2024). Global prevalence of male infertility and treatment access.