How a Genetic Variant Predicts Liver Damage from Chemotherapy in Colorectal Cancer Patients with Liver Metastases By Chloe Corey | October 2025
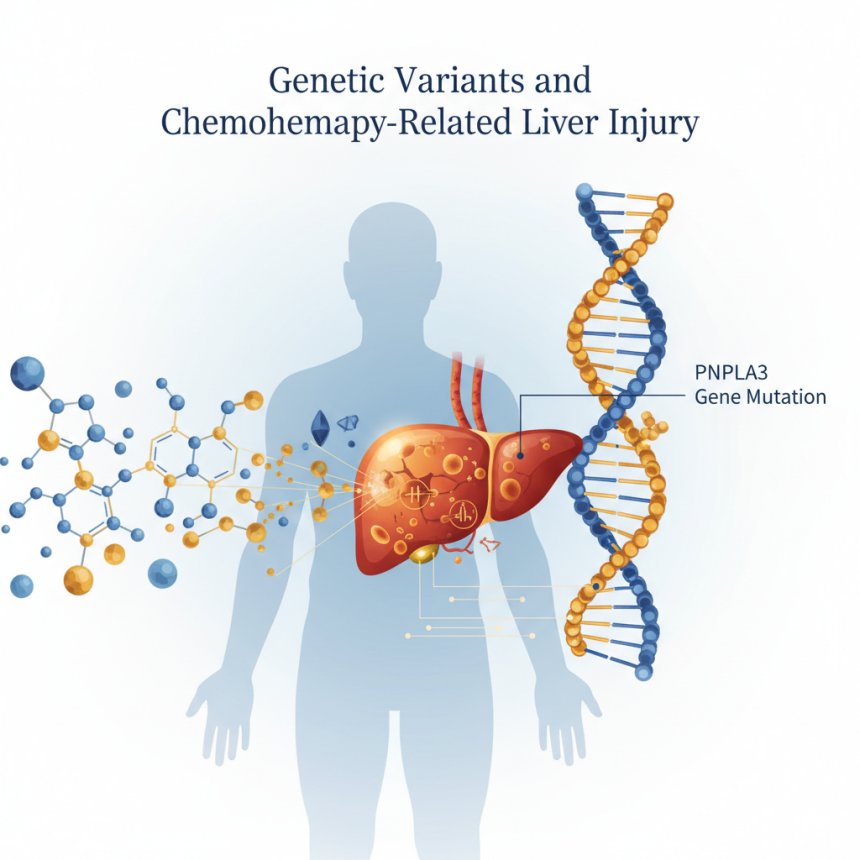
New research published in The Lancet eBioMedicine reveals that a genetic variant in the PNPLA3 gene significantly increases the risk of chemotherapy-related liver injury in patients with colorectal cancer liver metastases. Learn how genetic testing and personalized treatment can reduce complications and improve survival after liver surgery.

Introduction
Colorectal cancer remains one of the most common and deadly cancers worldwide. When the disease spreads to the liver — forming colorectal liver metastases (CRLM) — surgical removal of those metastases (hepatectomy) can offer the best hope for long-term survival.
To make surgery possible or more effective, many patients receive neoadjuvant chemotherapy (NAC) before surgery. Unfortunately, NAC can injure the liver — a condition called chemotherapy-associated liver injury (CALI). CALI can make surgery riskier and worsen long-term survival.
Why some patients develop severe CALI while others do not, even under similar chemotherapy regimens, has long puzzled clinicians. A groundbreaking 2025 study published in The Lancet eBioMedicine identifies a key piece of the puzzle: a genetic variant in the PNPLA3 gene that strongly predicts susceptibility to chemotherapy-induced liver damage.
Study Overview
Research Design
Researchers conducted an international retrospective study of 551 patients with colorectal cancer liver metastases who underwent neoadjuvant chemotherapy followed by hepatic resection.
In a genotyped subset of 149 patients, investigators tested for single nucleotide polymorphisms (SNPs) linked to liver disease. They found that one gene — PNPLA3 (patatin-like phospholipase domain-containing protein 3) — stood out.
Specifically, the rs738409 variant (coding for an I148M substitution) was significantly associated with increased liver injury after chemotherapy.
Measuring Liver Injury: The APRI + ALBI Score
To quantify liver injury, the team used a noninvasive composite marker combining two established clinical indices:
-
APRI (Aspartate Aminotransferase-to-Platelet Ratio Index): Indicates hepatic inflammation and fibrosis.
-
ALBI (Albumin-Bilirubin Score): Reflects liver synthetic function and biliary excretion capacity.
The researchers set a cutoff value of –2.46:
-
Patients with APRI + ALBI ≥ –2.46 were categorized as high-risk (injured).
-
Those with < –2.46 were low-risk (preserved function).
Key Findings
1. Liver Injury Correlates with Survival
Patients whose post-chemotherapy APRI + ALBI score was ≥ –2.46 had significantly worse overall survival (OS) after hepatectomy compared to those with lower scores.
-
Median OS:
-
Low-risk (score < –2.46): 46.1 months
-
High-risk (score ≥ –2.46): 34.3 months
(p = 0.027)
-
This demonstrates that chemotherapy-induced liver damage not only complicates surgery but also shortens survival.

2. PNPLA3 Variant Strongly Predicts Liver Injury
Among the 149 genotyped patients:
-
The PNPLA3 rs738409 variant (I148M) was strongly correlated with both chemotherapy-associated steatohepatitis (CASH) and increased hepatic fat content.
-
Strikingly, 100% of patients homozygous for the variant (carrying two copies) developed CALI (high-risk APRI + ALBI ≥ –2.46).
-
Heterozygotes (one copy) had intermediate risk, while wild-type patients were largely protected.
Thus, the variant is a dose-dependent genetic risk factor for chemotherapy-induced liver damage.
3. Impact on Long-Term Outcomes
The PNPLA3 genotype was indirectly predictive of overall survival, as it determined who developed significant CALI — which in turn was associated with worse postoperative outcomes.
The study highlights that liver injury during chemotherapy is not just a temporary complication; it has durable consequences for survival.
4. Population Differences
The PNPLA3 I148M variant’s frequency varies globally:
-
Japan: ~41% carry at least one copy
-
Peru: ~71% carry at least one copy
-
Europe: <10% carry at least one copy
Such variation may explain why the hepatotoxic effects of chemotherapy differ across ethnic and geographic populations.
Why This Gene Matters: The Biology of PNPLA3
The PNPLA3 enzyme regulates lipid metabolism in liver cells. The I148M mutation impairs lipid breakdown, causing fat accumulation (steatosis) and inflammation — a hallmark of nonalcoholic steatohepatitis (NASH).
During chemotherapy, drugs such as oxaliplatin and irinotecan impose oxidative stress on hepatocytes. In patients with the I148M variant, the already fatty, inflamed liver becomes far more susceptible to additional toxic damage — explaining the observed increase in CALI risk.
Clinical Implications
1. Genetic Risk Screening
-
Pre-treatment genotyping for PNPLA3 rs738409 could identify patients at higher risk for CALI.
-
This enables personalized chemotherapy planning — modifying drug choice, dose, or duration.
2. Dynamic Liver Monitoring
-
Regular monitoring using APRI + ALBI during chemotherapy can catch early signs of liver stress, allowing clinicians to adjust therapy before irreversible injury occurs.
3. Tailored Chemotherapy Regimens
-
Consider substituting or adjusting hepatotoxic agents like oxaliplatin or irinotecan in high-risk genotype carriers.
-
Allow longer “rest periods” before surgery for liver recovery.
4. Population-Specific Strategies
-
Populations with high PNPLA3 variant prevalence (e.g., East Asian, Latin American) may particularly benefit from genotype-guided chemotherapy management.
Limitations
-
Retrospective Design: Cannot prove causation, though associations are robust.
-
Subset Genotyping: Only 149 of 551 patients were tested.
-
Single Gene Focus: Other genetic and metabolic factors likely contribute to CALI risk.
-
Need for Prospective Validation: Future clinical trials must confirm benefits of genotype-guided approaches.
Future Directions
-
Prospective Trials — Validate PNPLA3-guided chemotherapy adjustments in multicenter studies.
-
Expanded Genetic Panels — Identify additional SNPs influencing hepatotoxicity.
-
Mechanistic Studies — Explore molecular pathways linking PNPLA3 to chemo injury.
-
Personalized Oncology Integration — Incorporate liver genetic risk screening into routine cancer care.
Conclusion

This landmark eBioMedicine study provides strong evidence that the PNPLA3 I148M variant significantly increases the risk of chemotherapy-induced liver injury and worsens survival in colorectal cancer patients with liver metastases.
By integrating genetic testing and dynamic liver monitoring into treatment planning, oncologists can move toward truly personalized chemotherapy — maximizing benefit while minimizing harm.
References
-
Corey, C. et al. PNPLA3 polymorphism worsens chemotherapy-associated liver injury and affects overall survival in colorectal cancer patients with liver metastasis undergoing hepatic resection. eBioMedicine (The Lancet), 2025. https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(25)00372-X/fulltext
-
Mayo Clinic News Network. New study links genetic variation to chemotherapy-related liver damage in patients with colorectal cancer liver metastases. September 2025. https://newsnetwork.mayoclinic.org/discussion/new-study-links-genetic-variation-to-chemotherapy-related-liver-damage-in-patients-with-colorectal-cancer-liver-metastases/
-
Inside Precision Medicine. Chemotherapy-Associated Liver Injury Elevated by Genetic Variant in CRLM. 2025. https://www.insideprecisionmedicine.com/topics/oncology/chemotherapy-associated-liver-injury-elevated-by-genetic-variant-in-crlm/
-
ResearchGate. PNPLA3 polymorphism worsens chemotherapy-associated liver injury... (Full-text summary, 2025). https://www.researchgate.net/publication/395537961_PNPLA3_polymorphism_worsens_chemotherapy_associated_liver_injury
-
Farrell, G. C., et al. PNPLA3 gene and liver disease: from genetics to mechanisms. Nature Reviews Gastroenterology & Hepatology. 2022;19(3):187–200. https://doi.org/10.1038/s41575-021-00553-w
-
Vauthey, J. N., et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. Journal of Clinical Oncology. 2006;24(13):2065–2072. https://doi.org/10.1200/JCO.2005.05.3074