Uncovering an “Unusual” Side Effect of Weight-Loss Drugs: What Doctors Need to Know About GLP-1s and Medical Imaging
New research reveals that weight-loss drugs like Ozempic and Wegovy may cause unusual PET-CT scan patterns, leading to potential misdiagnoses. Learn how healthcare professionals can recognize and manage this emerging side effect to ensure accurate imaging results and patient safety.

Introduction:
The rise of GLP-1 drugs—such as Ozempic, Wegovy, and Mounjaro—has revolutionized how we approach weight loss and type 2 diabetes management. According to a 2024 Kaiser Family Foundation poll, about one in eight U.S. adults have taken a GLP-1 medication.
But as their popularity soars, researchers are now identifying a new, unusual side effect that may not affect how patients feel—but could significantly impact how their medical imaging is interpreted.
Recent findings from Alliance Medical, presented at the Annual Congress of the European Association of Nuclear Medicine (EANM), revealed that GLP-1 drugs can cause abnormal uptake patterns during FDG PET-CT scans, potentially leading to misdiagnoses if healthcare professionals are unaware of a patient’s medication history.
Trump’s $150 Ozempic? Oz cautions it’s not a done deal, but patients and doctors say it could be a gamechangerU.S. President Donald Trump’s recent announcement that Ozempic — the popular diabetes and weight-loss drug — could soon cost as little as $150 a month has sent shockwaves through the pharmaceutical industry and sparked cautious optimism among patients and healthcare providers. Currently priced around $1,000 per month, Ozempic’s high cost has limited access for millions who could benefit from it. The proposed price reduction is part of Trump’s broader plan to lower prescription drug costs under the “Most Favored Nation” policy framework. However, CMS Administrator Dr. Mehmet Oz has cautioned that negotiations with manufacturers like Novo Nordisk are still ongoing and no final deal has been made. While markets reacted sharply — with shares of Novo Nordisk and Eli Lilly dropping — many doctors and patients hailed the potential shift as a game-changer that could make life-saving treatments more affordable. Experts, however, warn that policy and pricing logistics could take months to finalize. If implemented, the $150 Ozempic plan could redefine accessibility in the U.S. healthcare landscape, balancing innovation with affordability for millions struggling with diabetes and obesity. |
What’s Happening: How GLP-1 Drugs Interfere with PET-CT Scans
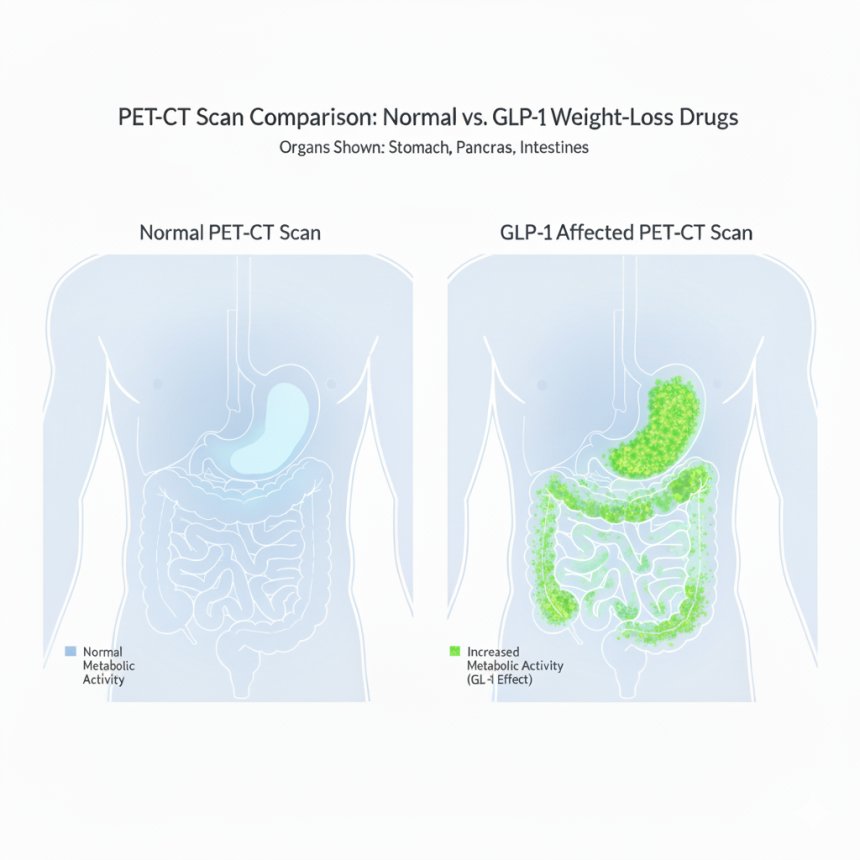
PET-CT (Positron Emission Tomography–Computed Tomography) scans are critical tools for diagnosing and tracking diseases like cancer. During these scans, patients receive an IV injection of fluorodeoxyglucose (FDG), a radiotracer that highlights cells consuming high amounts of glucose—often cancerous or inflamed cells.
However, patients using GLP-1 drugs (like semaglutide and tirzepatide) show unusual FDG uptake patterns, according to Dr. Peter Strouhal, Medical Director at Alliance Medical.
“We noticed unusual uptake in one of our patients on a GLP-1 agonist, which prompted a wider review across our network,” Dr. Strouhal explained.
“These altered patterns are increasingly common, yet there is currently no national or international guidance addressing this emerging issue.”
The concern is that these abnormal patterns may mimic disease, such as inflammation or tumor activity—leading to unnecessary follow-up tests, incorrect cancer staging, or delayed treatment.
Why It Matters: The Hidden Risk in the Scan Room
For oncologists and radiologists, context is everything. A PET-CT scan showing unexpected “hot spots” may trigger alarm bells for cancer recurrence or progression. Yet if these changes are drug-induced, acting on them could cause:
-
Unnecessary anxiety for patients
-
Additional imaging or biopsies
-
Incorrect treatment planning or cancer staging
-
Delays in proper care
Understanding the link between GLP-1 drugs and altered scan results is essential for accurate interpretation and optimal patient outcomes.
The Science Behind the Side Effect
GLP-1 receptor agonists work by stimulating insulin secretion, suppressing appetite, and slowing gastric emptying—mechanisms that aid in both weight loss and glucose control.
However, these same effects alter how tissues metabolize glucose, influencing FDG distribution during PET scans. Researchers believe that GLP-1 drugs may cause increased uptake in the stomach, intestines, and pancreas, regions that are already metabolically active, leading to confusing results.
Recommended Measures for Healthcare Professionals
To prevent misinterpretation and improve patient safety, experts recommend the following steps:
1. Document Medication History Thoroughly
Before any imaging, ask specifically about GLP-1 drug use (e.g., Ozempic, Wegovy, Mounjaro). Record the dosage, last administration date, and duration of therapy.
2. Communicate Between Teams
Radiologists, oncologists, and endocrinologists should share information to ensure that any unusual PET-CT findings are interpreted in the context of GLP-1 therapy.
3. Update Imaging Protocols
Hospitals and imaging centers should review PET-CT preparation guidelines to account for GLP-1-related uptake variations.
4. Consider Timing of Drug Administration
If medically appropriate, schedule scans several days after the last GLP-1 dose to reduce the impact of the drug on glucose metabolism during imaging.
5. Develop Clinical Guidelines
National and international imaging societies should create formal recommendations to guide radiologists and nuclear medicine specialists in identifying GLP-1-related FDG uptake patterns.
Impact and Future Implications
The discovery highlights how rapidly evolving medications can introduce unanticipated challenges in other areas of healthcare, such as diagnostics and imaging.
Dr. Strouhal emphasizes that recognizing GLP-1–related patterns is crucial:
“Recognizing the characteristic uptake associated with GLP-1 agonists helps avoid unnecessary anxiety and interventions, ensuring patients receive the right care, at the right time, without detours or doubt.”
As more people use GLP-1 drugs worldwide, the medical community must adapt imaging practices to ensure precision and patient safety.
Conclusion:
GLP-1 drugs have transformed obesity and diabetes care—but their influence doesn’t stop at the metabolic level. The discovery of unusual PET-CT scan patterns associated with these drugs serves as a reminder that innovation in one field can ripple through others.
For clinicians and imaging specialists, awareness and communication are key. By documenting GLP-1 use, updating imaging protocols, and collaborating across disciplines, healthcare professionals can avoid misdiagnoses and protect patients from unnecessary interventions.
As usage of GLP-1 agonists like Ozempic and Wegovy continues to climb, staying informed isn’t just good practice—it’s essential for safe, effective, and evidence-based care.
References:
-
Strouhal, P. et al. (2024). Abnormal FDG PET-CT Uptake Patterns in Patients on GLP-1 Agonists. Presented at the Annual Congress of the European Association of Nuclear Medicine (EANM).
-
Kaiser Family Foundation (2024). Public Opinion on GLP-1 Drugs for Weight Loss and Diabetes.
-
Cleveland Clinic (2024). FDG PET-CT: What It Is and How It Works.
-
American Association for the Advancement of Science (AAAS). (2024). GLP-1 Drugs May Interfere with Cancer Imaging Results.