Beyond Weight Loss: How the Gut Microbiome Is Redefining Long-Term Weight Maintenance and Personalized Nutrition
Long-term weight maintenance is no longer just about calories. Emerging research reveals how the gut microbiome influences metabolism, appetite, and weight regain. Discover how studies like the SWEET project are paving the way for microbiome-based personalized nutrition and sustainable weight management.
Introduction
For decades, the fight against obesity has been oversimplified into a single principle: eat less, move more. While caloric restriction leads to weight loss, keeping the weight off remains one of the greatest challenges in medicine. The body’s biological defenses—metabolic slowdown and increased hunger—often lead to inevitable regain.
Now, cutting-edge research is revealing a new frontier: the gut microbiome. This vast ecosystem of trillions of microorganisms not only impacts digestion and immunity but also appears to regulate how efficiently we burn calories, feel satiated, and store fat. Understanding and modulating the microbiome could revolutionize long-term weight management and enable personalized nutrition tailored to individual biology.
The Weight Loss Plateau: A Biological Tug-of-War
The weight loss journey typically follows a predictable curve: initial success, a frustrating plateau, and gradual regain. Contrary to popular belief, this is not simply a failure of discipline—it is a deeply rooted biological defense mechanism.
-
Metabolic Adaptation:
When weight is lost, resting energy expenditure (REE) declines more than expected. For every kilogram shed, REE decreases by roughly 20–30 kcal/day. -
Increased Appetite:
Hormonal changes—such as reduced leptin and elevated ghrelin—amplify hunger signals. Research suggests appetite rises by approximately 100 kcal/day per kilogram lost.
Thus, a person who loses 10 kg faces a double disadvantage: burning ~250 fewer calories daily while craving ~1000 more. This powerful metabolic resistance explains why sustaining weight loss requires more than willpower—it demands a deeper understanding of physiology and metabolism.
The Gut Microbiome: A New Frontier in Metabolic Health
The gut microbiome—comprising bacteria, viruses, and fungi—acts as a dynamic metabolic organ. It extracts nutrients, regulates inflammation, and produces key bioactive compounds such as short-chain fatty acids (SCFAs).
A healthy gut microbiome (known as eubiosis) promotes metabolic balance, whereas an imbalanced one (dysbiosis) contributes to insulin resistance, inflammation, and obesity. Factors such as diet, genetics, and environment shape each person’s microbial community, explaining why individuals respond differently to the same foods.
This variability is at the heart of personalized nutrition, where interventions are designed according to each individual’s unique microbial signature.
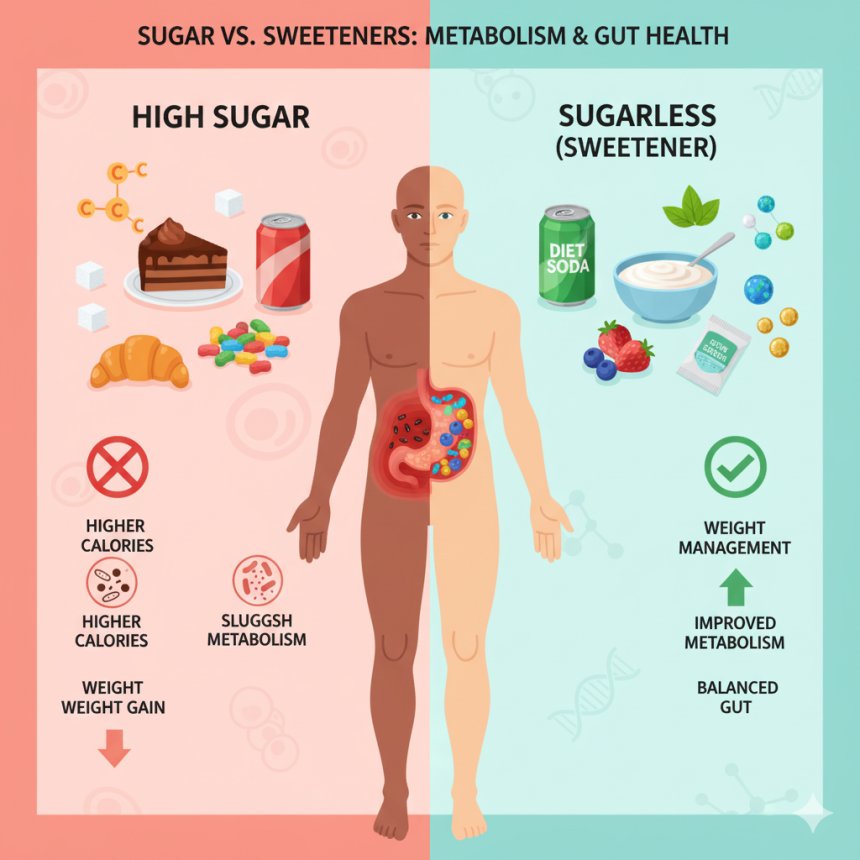
The SWEET Study: Linking Sweeteners, Gut Microbes, and Weight Maintenance
The landmark SWEET project (2025) provided one of the first large-scale demonstrations of how dietary choices reshape the microbiome and influence long-term weight outcomes.
Study Overview:
-
Participants: 300+ adults with overweight or obesity
-
Intervention: Replace sugar with sweeteners and sweetness enhancers (S&SEs) for 12 months
-
Comparison: Similar low-sugar diet with limited real sugar intake
Results:
-
S&SE users maintained 1.6 kg more weight loss after one year
-
Greater improvements in cholesterol levels and lipid metabolism
-
Distinct microbial shifts toward beneficial taxa, including Megasphaera, Prevotella, and Eubacterium eligens
These bacteria are renowned for producing SCFAs—notably butyrate and propionate—which enhance fat oxidation, suppress appetite via gut-brain signaling, and reduce inflammation.
Moreover, the study revealed that baseline microbiome composition could predict how well individuals maintained weight and improved blood sugar control—an early step toward microbiome-guided diet personalization.
Personalized Nutrition: Tailoring Diets to Microbial Signatures
A 2024 clinical trial on patients with type 2 diabetes and hyperlipidemia exemplified the promise of microbiome-driven nutrition.
Design:
-
30 participants randomized into:
-
Personalized Diet Group: Meal plans guided by gut microbiome sequencing
-
Control Group: Standard diabetic diet recommendations
-
Outcomes after 90 Days:
| Metric | Personalized Diet | Control Diet |
|---|---|---|
| HbA1c | ↓ from 8.30% → 6.67% | ↓ from 8.25% → 7.85% |
| CRP (Inflammation Marker) | ↓ 19.5% | ↓ 6.2% |
| Systolic BP | ↓ 5% | ↓ 2% |
| Microbiome Diversity | Significant increase | Minimal change |
The data reveal that microbiome-tailored diets not only improve metabolic outcomes but also enhance gut diversity—a hallmark of robust health.
A 2025 meta-analysis further confirmed that personalized nutrition based on microbial profiling leads to better glycemic control, lower post-meal glucose spikes, and reduced carbohydrate intake among individuals with metabolic disorders.
Clinical Implications: Shifting the Paradigm
-
Reframing Weight Regain:
Clinicians must help patients understand that post-diet weight rebound is biologically driven, not a moral failing. This fosters compassion and long-term engagement. -
Integrating Microbiome Science:
Referrals to qualified dietitians with microbiome expertise can help patients with obesity, diabetes, or metabolic syndrome receive personalized dietary interventions that work with, not against, their biology. -
Future-Proofing Clinical Practice:
As technology advances, metagenomic testing and machine learning models will allow practitioners to predict individual responses to specific nutrients or sweeteners—ushering in a new era of precision nutrition.
Conclusion
Long-term weight management is more than a matter of calorie arithmetic—it’s a biological negotiation between the body, the diet, and the trillions of microbes that inhabit our gut.
Evidence from the SWEET study and other clinical trials reveals that modifying the microbiome through dietary strategies—such as sweetener substitution or microbiome-guided meal planning—can significantly improve weight maintenance, metabolic resilience, and inflammation control.
The future of nutrition lies in personalization: harnessing the microbiome’s unique blueprint to craft dietary interventions that align with each individual’s metabolism. In doing so, we move closer to achieving what has long eluded public health—sustainable, biologically informed weight management.
References
-
Blaak, E. et al. (2025). Effect of sweeteners and sweetness enhancers on weight management and gut microbiota composition: The SWEET Study. Nature Metabolism.
-
Zeevi, D. et al. (2024). Personalized nutrition by prediction of glycemic responses. Cell.
-
Turnbaugh, P. J., & Gordon, J. I. (2023). Microbiome and energy balance in obesity. Science.
-
DMSO Review (2025). Systematic review of personalized nutrition and metabolic outcomes. Diabetes, Metabolism, and Obesity.