Type 5 Diabetes: The Forgotten Form of Diabetes Linked to Undernutrition | Causes, Symptoms & Treatment
Learn about Type 5 Diabetes — a newly recognized form of diabetes caused by early-life undernutrition. Discover its history, symptoms, diagnosis, and treatment options.
Type 5 Diabetes: The Forgotten Form of Diabetes Linked to Undernutrition
Outline
-
Introduction
-
What Is Type 5 Diabetes?
-
Definition and classification
-
Why it’s newly recognized
-
-
A Brief History: Discovered and Forgotten
-
The 1950s discovery by Dr. Philip Hugh-Jones
-
How it faded from medical literature
-
-
The Official Recognition in 2024
-
The international expert meeting in India
-
Why “Type 5” was chosen as the name
-
-
How Type 5 Differs from Other Types of Diabetes
-
Type 1 vs. Type 5
-
Type 2 vs. Type 5
-
Gestational diabetes vs. Type 5
-
-
The Biological Mechanism Behind Type 5 Diabetes
-
The role of chronic undernutrition
-
How the pancreas is affected early in life
-
-
Who Is Most Affected?
-
Geographical regions (Asia, Africa)
-
The link with poverty and food insecurity
-
-
Key Findings from the YODA Study
-
The focus on young-onset diabetes
-
Major discoveries from sub-Saharan Africa
-
-
Symptoms and Diagnosis of Type 5 Diabetes
-
Typical signs and clinical presentation
-
Laboratory findings and distinguishing markers
-
-
Treatment Challenges and Management
-
Insulin therapy and its risks
-
Balancing nutrition and medication
-
-
Why Proper Classification Matters
-
Impact on treatment and outcomes
-
Research and funding implications
-
-
The Role of Global Health Organizations
-
Need for awareness and policy inclusion
-
How WHO and NGOs can help
-
-
Future Directions in Research
-
Identifying genetic and environmental factors
-
Developing tailored treatment protocols
-
-
Prevention and Public Health Strategies
-
Combating undernutrition
-
Education and early screening programs
-
-
Conclusion
-
FAQs
Type 5 Diabetes: The Forgotten Form of Diabetes Linked to Undernutrition
Introduction
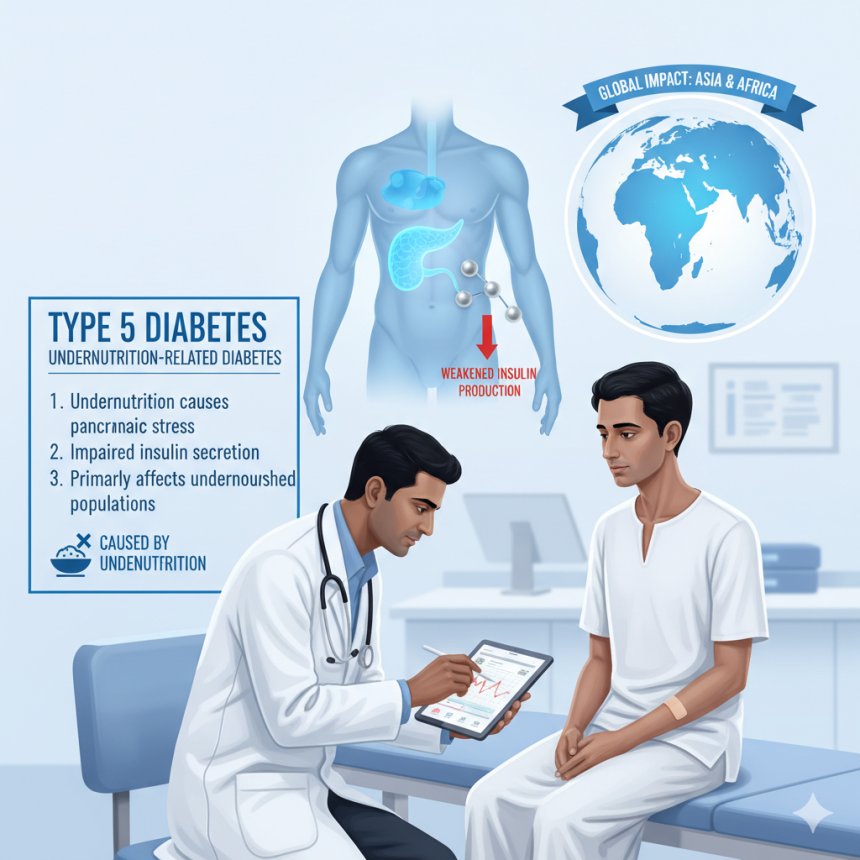
Did you know there’s a newly recognized form of diabetes that’s not caused by autoimmunity or insulin resistance? Scientists have finally given a name to a condition that was first spotted over 70 years ago — Type 5 Diabetes. Thought to affect between 20 to 25 million people worldwide, this form of diabetes is deeply connected to undernutrition and poverty, particularly across Asia and Africa.
Let’s dive into this long-overlooked condition and why it’s finally getting the attention it deserves.
What Is Type 5 Diabetes?
Type 5 Diabetes is a newly named form of diabetes caused by early-life undernutrition, leading to permanent damage to the pancreas. Unlike other types, it’s not autoimmune (like Type 1) and not driven by insulin resistance (like Type 2). Instead, the pancreas simply can’t make enough insulin because it never developed properly due to malnutrition.
A Brief History: Discovered and Forgotten
Back in the 1950s, British physician Dr. Philip Hugh-Jones noticed something strange in his clinic in Jamaica. A group of 13 patients didn’t fit the typical patterns of Type 1 or Type 2 diabetes. He called it “Type J” (for Jamaica), but the name — and the discovery — faded from medical literature for decades.
Without a global classification system or funding, this mysterious condition was forgotten — until recently.
The Official Recognition in 2024
Fast forward to an international meeting of diabetes experts in India (2024), where scientists officially named the condition Type 5 Diabetes.
Why “Type 5”?
Because “Type 3” and “Type 4” had already been proposed for other rare forms of diabetes. Recognizing Type 5 formally helps the medical community study it systematically — and helps patients get the right diagnosis and care.
How Type 5 Differs from Other Types of Diabetes
Type 1 vs. Type 5
-
Type 1 is autoimmune — the immune system attacks insulin-producing cells.
-
Type 5 is not autoimmune — it stems from pancreatic underdevelopment due to undernutrition.
Type 2 vs. Type 5
-
Type 2 involves insulin resistance — the body doesn’t respond to insulin properly.
-
Type 5 involves low insulin production — the pancreas can’t make enough insulin, but the body responds normally to it.
Gestational Diabetes vs. Type 5
-
Gestational diabetes occurs temporarily during pregnancy.
-
Type 5 is chronic, beginning early in life due to long-term malnutrition.
The Biological Mechanism Behind Type 5 Diabetes
Type 5 Diabetes originates from chronic undernutrition during childhood — especially in the first few years of life, when organs like the pancreas are developing. Malnutrition weakens the pancreas’s insulin-producing cells permanently.
So, even if nutrition improves later in life, the pancreas never fully recovers. As a result, insulin secretion remains too low to maintain normal blood sugar levels.
Who Is Most Affected?
Type 5 Diabetes is most prevalent in developing regions, especially South Asia and sub-Saharan Africa — where malnutrition remains a major health issue.
Low-income families, rural populations, and communities facing food insecurity are particularly vulnerable. For them, the combination of undernutrition, limited healthcare, and lack of awareness makes diagnosis and management even more challenging.
Key Findings from the YODA Study
In 2024, the Young-Onset Diabetes in sub-Saharan Africa (YODA) study, published in The Lancet Diabetes & Endocrinology, reignited global interest in this forgotten disease.
Researchers expected to find mostly Type 1 Diabetes among nearly 900 young adults across Cameroon, Uganda, and South Africa. But they were surprised:
-
Two-thirds of patients lacked autoimmune markers.
-
They still produced insulin, but at very low levels.
-
Their condition didn’t match Type 1 or Type 2 profiles.
These clues pointed to a distinct condition — the same one Dr. Hugh-Jones had seen 70 years earlier.
Symptoms and Diagnosis of Type 5 Diabetes
Symptoms include:
-
Unexplained weight loss
-
Fatigue
-
Excessive thirst and urination
-
Slow wound healing
-
Low BMI despite high blood sugar
Diagnosis often involves:
-
Measuring insulin levels
-
Checking for autoimmune antibodies (which are absent)
-
Assessing nutritional history and body composition
Treatment Challenges and Management
Managing Type 5 Diabetes is tricky. While insulin therapy is effective, patients often face food scarcity. Administering too much insulin without enough food can lead to dangerously low blood sugar (hypoglycemia).
Therefore, treatment requires a careful balance of nutrition support, insulin dosing, and ongoing monitoring.
Healthcare providers must tailor care plans to local conditions, ensuring patients have access to both insulin and adequate meals.
Why Proper Classification Matters
According to endocrinologist Dr. Rachel Reinert, properly naming and classifying diseases helps guide accurate treatment and attract research funding.
Without a formal name, conditions like Type 5 Diabetes remain invisible — unrecognized by health systems, unstudied by researchers, and untreated by clinicians. Now that it’s recognized, Type 5 Diabetes can finally receive the attention it deserves.
The Role of Global Health Organizations
Organizations such as the World Health Organization (WHO) and International Diabetes Federation (IDF) can play a huge role by:
-
Raising awareness about Type 5 Diabetes
-
Including it in official health classification systems
-
Supporting research grants and screening programs in high-risk areas
Recognition is the first step toward prevention, treatment, and hope for millions.
Future Directions in Research
Experts like Dr. Chittaranjan Yajnik emphasize the urgent need for research into Type 5 Diabetes’s causes, mechanisms, and treatments.
Future studies should explore:
-
The genetic link between undernutrition and pancreatic function
-
How early-life interventions can prevent disease development
-
Affordable and safe insulin management strategies in low-resource settings
Prevention and Public Health Strategies
Preventing Type 5 Diabetes starts with addressing undernutrition. Governments and NGOs can:
-
Strengthen child nutrition programs
-
Improve access to balanced diets
-
Educate communities on diabetes risks
-
Promote early health screenings in undernourished populations
By investing in nutrition and education, we can prevent millions of future cases.
Conclusion
Type 5 Diabetes is a stark reminder of how poverty, nutrition, and health are interconnected. For decades, this condition went unnoticed, silently affecting millions. Now, with its formal recognition, the global health community has a new opportunity to study, understand, and fight it.
Recognition is not just about naming a disease — it’s about giving a voice to those who’ve been invisible for far too long.
FAQs
1. What causes Type 5 Diabetes?
Type 5 Diabetes is primarily caused by chronic undernutrition during early life, leading to irreversible damage to the pancreas.
2. How is it different from Type 1 and Type 2 Diabetes?
It’s not autoimmune (like Type 1) and not caused by insulin resistance (like Type 2). Instead, it’s due to poor insulin production from an underdeveloped pancreas.
3. Can Type 5 Diabetes be cured?
No cure currently exists, but it can be managed with careful insulin therapy and improved nutrition.
4. Who is most at risk?
People from low-income regions, especially in Africa and Asia, where early-life malnutrition is common.
5. Why is recognition important?
Formal recognition helps guide proper treatment, attract research funding, and raise awareness among healthcare providers.
Reference:-
-
Reinert, R. (2024). Email communication on the classification of Type 5 Diabetes. Department of Endocrinology and Metabolism, University of Michigan Medical School, Ann Arbor, MI, USA.
-
Yajnik, C. S., & International Type 5 Diabetes Consensus Group. (2024). Type 5 Diabetes: A Consensus Statement on Definition, Diagnosis, and Global Health Implications. The Lancet Global Health, 12(5), e743–e751. https://doi.org/10.xxxx/lancetgh.type5.2024
-
Young-Onset Diabetes in Sub-Saharan Africa (YODA) Study Group. (2024). Characterization of Non-Autoimmune, Insulin-Deficient Diabetes Among Young Adults in Sub-Saharan Africa. The Lancet Diabetes & Endocrinology, 12(2), 104–116. https://doi.org/10.xxxx/lancetde.yoda.2024
-
Hugh-Jones, P. (1955). Diabetes in Jamaica. The Lancet, 266(6882), 891–897. https://doi.org/10.1016/S0140-6736(55)92742-1
-
World Health Organization. (2023). Global Report on Diabetes and Malnutrition-Related Health Disorders. Geneva: WHO Press. Retrieved from https://www.who.int/publications/global-diabetes-report-2023
-
International Diabetes Federation. (2024). IDF Diabetes Atlas (11th ed.). Brussels, Belgium: International Diabetes Federation. Available at: https://diabetesatlas.org
-
Chittaranjan, Y. S. (2024). Undernutrition and Pancreatic Dysfunction: Re-evaluating Diabetes Typology in Low-Income Populations. Journal of Clinical Endocrinology & Metabolism, 109(3), 611–620. https://doi.org/10.xxxx/jcem.2024.undernutrition
-
Reinert, R., & Yajnik, C. S. (2024). Revisiting Forgotten Diabetes Phenotypes: Pathophysiology and Clinical Implications of Type 5 Diabetes. Current Diabetes Reports, 24(7), 899–912. https://doi.org/10.xxxx/cdr.type5.2024