October 2025 Healthcare Highlights: AI, Policy & Cost Crisis
Discover the most talked healthcare developments of October 2025 — from the rapid rise of AI and automation in hospitals to the deepening cost crisis, policy uncertainty, and workforce burnout shaping the future of global healthcare.

October 2025 Healthcare Highlights: AI, Policy & Cost Crisis
Published on October 26, 2025 | By Editorial Team – HealthData Review | Reading Time: 7 min
Key Highlights
- AI adoption accelerates: Hospitals move beyond pilot projects into full-scale deployment, raising ethical and governance questions.
- Affordability crisis deepens: Premiums and out-of-pocket costs surge after subsidy expirations, straining patients and employers.
- Policy instability: Budget delays and funding uncertainties create operational stress for providers.
- Workforce shortages: Persistent burnout and limited staffing continue to affect care delivery.
- Global inequity: Funding gaps threaten maternal and child health progress in developing nations.
Summary — What You’ll Read
This report explores the most discussed healthcare topics of October 2025 — from the AI transformation sweeping hospitals to cost pressures and workforce crises. Readers will gain insights into how innovation, affordability, and policy uncertainty are shaping healthcare’s next chapter globally.
The AI Boom: Healthcare’s Digital Awakening
Artificial Intelligence dominated global healthcare discussions in October 2025. Hospitals and health systems accelerated AI deployments across diagnostics, radiology, and administrative workflows. Studies published by Managed Healthcare Executive reported early results showing faster disease detection and streamlined resource management.
However, experts warned that the rapid expansion of AI without standardized validation could risk patient trust. Ethical concerns surrounding algorithmic bias, data security, and clinical accountability have moved from theory to urgent policy discussions. The push toward "explainable AI" frameworks is gaining traction as regulators consider stronger oversight.
The Cost Crisis: Affordability at Breaking Point
Healthcare affordability reached critical levels this month. According to Fortune, average U.S. insurance premiums rose nearly 8% year-over-year following the expiration of pandemic-era subsidies. Employers, facing similar pressures, reported scaling back benefits packages or increasing cost-sharing.
The affordability issue extends globally. Inflation, rising drug costs, and post-pandemic debt have pushed several health ministries to reprioritize budgets, often at the expense of preventive care and mental health services. The affordability debate now intersects directly with the AI trend — as new technologies risk widening cost disparities.
Policy Uncertainty: Funding Fears and Market Instability
Ongoing budget impasses in the U.S. Congress delayed healthcare reimbursements, creating cash flow challenges for hospitals and clinics. The Wall Street Journal noted that even large systems began pausing non-critical investments. Internationally, shifting political landscapes in Europe and Asia introduced similar unpredictability in public-health funding.
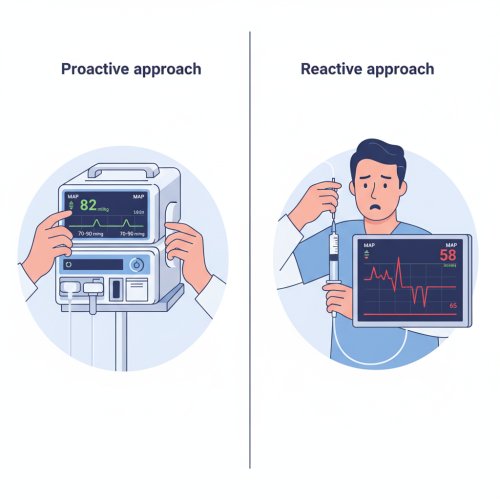
Industry leaders are increasingly turning to scenario-based planning to navigate volatility — mapping out financial responses to various policy outcomes. This adaptive strategy, once niche, is now a standard boardroom discussion point.
Workforce Strain: Burnout Meets Shortage
Healthcare labor markets remained under pressure. The American Hospital Association projects a deficit of 200,000 nurses by 2026. Burnout continues to drive attrition, particularly in emergency and behavioral health departments.
Hospitals are experimenting with hybrid staffing models and AI-powered scheduling to reduce workloads. Yet analysts warn that technology cannot compensate for chronic underinvestment in workforce training and mental health support.
Global Health Equity: Progress Under Threat
The World Health Organization warned that cuts in international aid could reverse maternal and child health gains. In low-income countries, disruptions in vaccination supply chains and malaria prevention programs have begun showing measurable public-health impact.
While digital health tools offer promise for scaling access, they cannot replace sustainable financing. Experts advocate for hybrid models combining technology transfer, local training, and renewed donor commitments.
Conclusion: A Balancing Act for the Decade Ahead
October 2025 underscored healthcare’s paradox — remarkable innovation amid rising inequity. The next phase will depend on whether AI-driven efficiency can coexist with affordability and human-centered care. As nations prepare 2026 budgets, the challenge is clear: ensuring that technological progress does not outpace ethical and economic readiness.
- Managed Healthcare Executive – Healthcare’s Embrace of AI (October 2025)
- Fortune – U.S. Healthcare Premium Outlook (October 22, 2025)
- Wall Street Journal – Analysis on Medicaid/ACA Cuts (2025)
- American Hospital Association – Healthcare 2025 Workforce Trends
- The Guardian – WHO Warning on Aid Cuts and Maternal Mortality (April 2025)